[MA 2018 038] When does depression become a killer?
Amsterdam UMC, location AMC, Department of Medical Psychology
Proposed by: Dr. Jos Bosch [j.a.bosch@uva.nl]
Introduction
Cardiovascular disease the most prevalent cause of mortality. Meta-analyses consistently show that among individuals with cardiac problems, depression (i.e., persistent sad mood or loss of interest) more than doubles the risk of having a fatal or non-fatal cardiac event (e.g., heart attack) within 24 months [1]. The American heart association has therefore issued an advisory in which it recommends that all admitted cardiac patients are routinely screened for depression [2]. However, it also appears that depression does not similarly increase cardiovascular risk for all patients, i.e., the association is heterogeneous. Likely, therefore, depression exerts its cardio-toxic effects in combination with other factors. These factors have yet to be identified, which is the purpose of the current project. Usually such analyses are hypothesis-bases, but this approach has thus far been unsuccessful in providing strong answers. Therefore, in this project we specifically take a data-based approach. We want to determine if there are distinctive clusters or profiles of risk factors that, in combination with depression, predict mortal or non-mortal cardiac events (e.g., heart attacks, cerebrovascular events).
Description of the SRP Project/Problem
Problem: To identify for whom depression may become a deadly disease
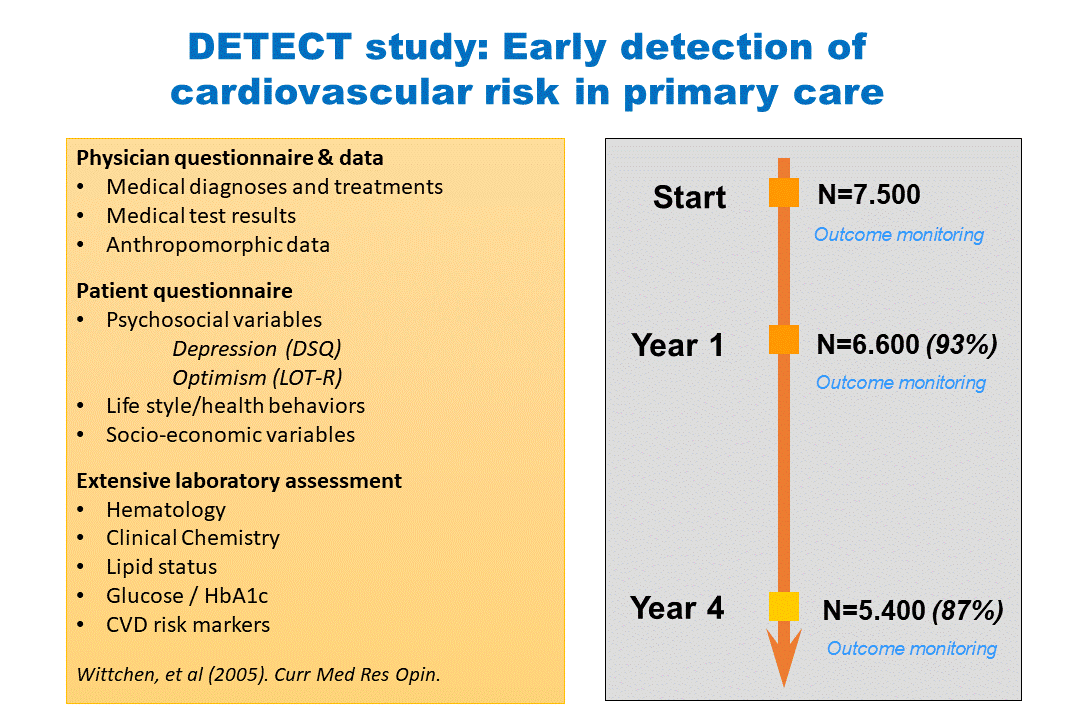
Data: The available data are from a longitudinal study with 7,500 patients in general practice (“Early detection of cardiovascular risk in primary care” DETECT). From these patients measurements were taken at three time pints (at 0, 1 and 4 years), whereby at each time point a very large number of medical, biological, and psychological variables were measured. See Figure.
Research Objectives
• Which combination of factors predict if depression increases likelihood of:
o mortality,
o myocardial infarctions
o improvement of worsening of diabetes (as a main cardiovascular risk factor)?
• Is there an interaction-effect, i.e., can we identify the context (cluster of risk factors) in which depression is a maximum risk factor?
Methods
We investigate if (i) mixed-effects logistics regression, (ii) generalized estimating equation (GEE) logistic regression, (iii) factor analysis or (iv) machine learning can answer the posed research questions.
Results
• Specification of associations of medical, biological and psychological factors in relation to depression, mortality, myocardial infarctions or diabetes.
• Model performance and validation statistics.
Time period
Eight months.
References
[1] Meijer, A., Conradi, H. J., Bos, E. H., Thombs, B. D., van Melle, J. P., & de Jonge, P. (2011). Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis of 25 years of research. General Hospital Psychiatry, 33(3), 203-216. DOI:10.1016/j.genhosppsych.2011.02.007Lichtman, J. H., Bigger, J. T., Jr.,
[2] Blumenthal, J. A., Frasure-Smith, N., Kaufmann, P. G., Lesperance, F., . . . American Psychiatric, A. (2008). Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation, 118(17), 1768-1775. doi:10.1161/CIRCULATIONAHA.108.190769